Quick Hit Summary
Many individuals suffer from chronic connective tissue injuries such as torn ligaments, damaged tendons and/or degenerating cartilage. Although it has been around for 100's of years, a "new" treatment technique, referred to as prolotherapy, has been promoted by some physicians as effective non-surgical technique to heal these injuries. It purportedly accomplishes this by increasing inflammation (and resulting healing response) in select regions of damaged tissue. Thus, strengthening and removing laxity in the targeted connective tissue areas. In Part II of this series, we examine the effects of traditional prolotherapy healing agents such as dextrose and sodium morrhuate. Various reports of beneficial effects of prolotherapy on ankle/Achilles, knee, pelvis/low back and elbow pain have been noted in the literature; Despite the positive effects reported, to date, some may argue that it still lacks “strong” evidence as most of it has been in the form of case reports and non-blinded studies. That said, I do believe there is enough preliminary evidence for one to pursue prolotherapy under the right conditions… especially when the alternative is going under the knife for surgery!
Prolotherapy Series
This is the 2nd part of our Prolotherapy Series. This collection of articles is focusing in on an emerging therapeutic technique in sports medicine as well as general orthopedic health known as prolotherapy. In all, there will be 3 parts to this series:
- Prolotherapy Part III: Proliferants 2.0 – Human Growth Hormone, Platelet Rich Plasma, and Orthokine/Regenokine
Recap of Part I & Confusion Clear Up

Figure 1. If you have the misfortune of suffering a connective tissue injury and laying in surgical operating room doesn't sound appealing, you may be interested in exploring a few prolotherapy treatments. Image source.12
Chronic vs. Acute Inflammation I want to stress that prolotherapy works via acute inflammation in specifically targeted tissues. Acute inflammation leads to a normal healing cascade, resulting in tissue that is stronger than it was prior to becoming inflamed. Example – muscle gets inflamed & then stronger following an exercise session. This varies considerably to the chronic inflammation that is caused by bones improperly rubbing against each other in a joint due to connective tissue laxity and/or poor biomechanics. In the latter situation, the tissue never gets a chance to heal, thus leading to degeneration.
In Part I of our series, we were introduced to prolotherapy, an injection based therapy which purportedly heals connective tissue injuries such as torn ligaments, damaged tendons and/or degenerating cartilage. As we saw, various animal studies have examined the mechanistic route in which prolotherapy may benefit those suffering from connective tissue injuries. Although some interesting results were shown, caveats were present making it impossible to form firm conclusions; Namely, different solutions were used, only 1 study actually involved injured tissue (and that was an acute injury vs. chronic injury), etc, etc.
Our introduction to prolotherapy likely grabbed your attention, but let's be honest, who really cares what happens in animals if the results fail to translate over to you & I, right?! Thus, let's get this show on the road and get to answering today's burning question – "Is prolotherapy a legit treatment for connective tissue injuries?"
We will attempt to answer this question to the best of our ability by focusing our attention on research done in the following body parts:
- Ankle/Achilles
- Knee
- Groin/Pelvis/Low Back
- Elbow
Prolotherapy Research using Traditional Proliferants – Human Based Research
As you'll see in the research that follows, there have not been many tightly controlled randomized clinical control studies in humans which have used prolotherapy. Rather, with a few exceptions, we're mostly left with case studies, single blinded and similar study designs, which as discussed in Research 101 are, from a scientific perspective, far from the gold standard double blinded placebo controlled randomized clinical control study. Thus, caveats are present with all the studies discussed below and I'm WELL aware of them… With that being said, let's look at the research, starting from the Achilles tendon/ankle before proceeding north to the knee, pelvis/low back, before finally ending with the elbow.
Prolotherapy for Achilles Tendon Related Pain/Talofibular Ligament Sprain of Ankle
One case study has been noted in the literature regarding the ligaments that cross the ankle joint1. In it, Dr. Bradley Fullerton treated a 17 year old softball pitcher who came to him following a motor vehicle accident that resulted in, according to the MRI report, "chronic appearing tear of the anterior talofibular ligament” (ATFL)… with associated fibrosis… probable tear of the calcaneal fibular ligament, partial tear involving the deep fibers of the deltoid ligament…"
After her injury and prior to starting prolotherapy, she had underwent 6 weeks of physical therapy "with minimal improvement" and still had "weakness, pain and instability" at the onset of the prolotherapy treatments which began 4.5 months following the initial injury1. Two dextrose based treatments were conducted over a ~4 month period; pain and instability decreased; ultrasound images showed ordered fiber orientation vs. random scar tissue growth. She then decided to momentarily stop injections as she was having minimal issues and the softball season had started up. A final injection, (for a total of 3 injections) was conducted at the 6 month mark. A MRI ordered 10 months following the initial MRI indicated "…enlargement and fibrosis of the anterior talofibular ligament is noted consistent with healing of a prior ligament tear…", "… A prior partial tear of the deltoid ligament has healed without evidence of abnormality…"
To my knowledge, there has been 1 randomized clinical trial, conducted by Yelland et al, which examined the effects of prolotherapy on Achilles tendon related pain.2 In their study, 43 individuals (age range – 40 to 58 years), who had been suffering from Achilles tendonosis for at least 4.5 months, were separated into 3 separate groups:
- Eccentric Loading Rehab (Straight knee and bent knee eccentric calf raises); 12 week program
- Prolotherapy (dextrose solution given at weekly intervals for up to 12 weeks or until patient felt they were “healed”)
- Combined (Eccentric + Prolotherapy)

Figure 2. Number of successful outcomes following 3 different therapy techniques. Data adapted from Yelland et al.2 Image created by Sean Casey.
A global assessment of pain, stiffness, activities of daily life and sporting activity were assessed 1.5, 3, 6 and 12 months following the start of each treatment using the VISA-A questionnaire.2 As stated by the researchers, 20 point increases in VISA-A scores are noted as successful clinical outcomes (ie – therapy proved effective). As seen in Figure 2, at 3, 6 and 12 months following first treatment, no differences existed between groups. However, during the first 6 weeks, the combined treatment group had significantly more “successful outcomes” than the eccentric only group. When directly assessing individual components such as subjective pain, stiffness and limitation in activities (via a 1-10 scale), the prolotherapy and combined group had slightly faster improvements vs. the eccentric only group. Thus, researchers stated that all three approaches proved to have successful long term outcomes. However, the addition of prolotherapy to the eccentric exercise program may speed up the rate of healing vs. eccentric exercise alone. Additionally, prolotherapy on its own was just as effective for reducing Achilles related pain as eccentric focused exercise.
A caveat with Yelland et al's study worth mentioning is that attention bias is a confounding factor; those in the prolotherapy groups had ~ 9 sessions with the practicing prolotherapist vs. the eccentric training groups which had only 3 supervised visits. Additionally, those in the combined group had been experiencing Achilles pain for a shorter time period than those in the prolo and exercise only groups which may explain why they “bounced back” quicker.
Prolotherapy for Knee Related Pain
There have been various case studies which have examined the effects of prolotherapy on knee related pain. Positive effects of dextrose based prolotherapy have been documented by Fullerton when used for patellar tendonopathy as well as meniscus tears with accompanying improvements on MRI and Ultrasound imaging.1
Grote et al. also reported on the positive effects of prolotherapy on an 18 year old active female who suffered, based off MRI results "extensive high-grade partial tear or complete tear" of her Anterior Cruciate Ligament (ACL).3 She declined surgery and 22 weeks later began prolotherapy. At the onset of treatments, she reported significant knee dysfunction that limited normal daily living activities as well as ambulated "poorly without crutches". Over the course of 15 weeks, the patient received 7 prolotherapy treatments that were conducted every 1-4 weeks with solutions that contained one or more of the following proliferants: dextrose, sodium morrhuate, phenol-quinine-urea and/or pumice. By week 5 of treatment, she was given the "OK" to start light bicycling, perform 1/3 squats and light leg extensions. By week 10, the patient reported that she was "back to 80% of baseline." She was able to walk, use stairs, bike (30 min/day) and perform leg extensions (3×8) with 7 lb (3 kg) pain free. By week 15 of treatment (37 weeks post injury), she was "very satisfied with her care" and released to perform recreational sports. MRI taken at this time showed a "well healed, relatively homogeneous ACL… a healing chronic ACL tear."
Switching gears slightly, the effects of prolotherapy on knee osteoarthritis (KOA) have also been examined by research teams. Dumais et al examined the effects dextrose based prolotherapy on 36 individuals (~56 years old) who had been diagnosed with KOA for at least 6 months and still suffered pain. On a 1-4 grading scale with 4 being the worst, 21 of the study's participants had grade 3 osteoarthritis and 10 had grade 4 osteoarthritis.4 All individuals were given a "home based exercise program for 32 weeks" that focused on strengthening the quadriceps muscles; These exercises were then reviewed with a physiotherapist every 4 weeks. In addition, individuals were randomized into 2 groups:
- Group A: Received prolotherapy at weeks 0, 4, 8, 12
- Group B: Received prolotherapy at weeks 20, 24, 28, 32
Using the WOMAC assessment, a clinically accepted means to measure osteoarthritis symptoms, the researchers found that despite following the exercise program (albeit not the "best" rehab program in my opinion) throughout the entire 32 week time period, statistically significant improvements in WOMAC scores occurred only during the prolotherapy injection time period. These improvements persisted throughout the remainder of the trial for Group A which had the injections during the first 12 weeks. Over the course of the entire trial, Group A increased WOMAC scores by 47% and Group B had a 36% improvement. For reference, it's been stated that a ~ 25% increase in WOMAC scores is considered a clinically significant improvement.5

Figure 4. Improvements in WOMAC assessment scores with time. Data adapted from Rabago et al.5 Image created by Sean Casey
In a different study, Rabago et al. also assessed the affects of prolotherapy on improvements in WOMAC scores in 36 individuals (mean age – 60 years old) who had moderate to severe KOA and had "failed one or more conservative measures" for treatment.5 All individuals received dextrose based prolotherapy treatments at weeks 1, 5, 9. Optional treatment sessions were conducted at weeks 13 and 17. The average number of treatments per individual was 4.3 sessions. WOMAC assessments were given at 5 different time points over the course of the year that followed; As seen in Figure 4, there was a statistically significant 36% improvement in WOMAC scores from baseline till studies end (again exceeding the 25% threshold improvement noted as being clinically significant). As you’ll notice, at week 24 there was a dip in scores. Rabago et al hypothesized this occurred:
“…perhaps because some participants overused their knees following substantial improvement in knee pain at one or more time points in the study. These results may therefore underestimate the potential effect of prolotherapy in patients who adhere to recommendations for a gentle return to activity or sport following prolotherapy."5
Unfortunately the studies completed by Dumais et al and Rabago et al, did not include post treatment follow-up MRI's, X-Rays or similar medical imaging to better understand the mechanism potentially behind observed improvements. Remember, as I mentioned in Part I, there is some theories that the pain relief experienced following prolotherapy may be related to it's ability to alter pain signals sent via nerves surrounding the given area.
Prolotherapy for Groin/Pelvis/Back Related Pain
The physical therapy protocol for the 72 athletes prior to inclusion into the study by Topol & Reeves involved "a minimum of 1 mo of rest from running or jogging with core strengthening and stretching, followed by a minimum of 1 mo of graded activity reintroduction." Most of the athletes had also received deep tissue massage during this initial time period as well.
In a case series presented by Topol & Reeves, the effects of dextrose based prolotherapy on groin pain in 72 elite athletes (mostly rugby and soccer athletes), who failed to experience any significant improvement following 2 months of physical therapy alone (see sidebox), was presented.6 Mean history of groin pain prior to enrolling in study was 11 months (range 3-60 months). Using a dextrose based solution, prolotherapy injections were given at 4 week intervals until improvements hit a plateau. During the time period in which they were treated, athletes were instructed not to take any anti-inflammatory medications such as ibuprofen, etc. Additionally, they were instructed to continue with their core/groin rehab exercises and to work back into sport play as allowed by their body's pain levels.
Upon review of the data, Topol & Reeves found that upon starting up with prolotherapy, following a minimum of 2 months of failing to see improvements with physical therapy alone, most athletes responded well. 66 of the 72 individuals were able to return to full sport activity. Additionally, 77% of injured athletes only needed 3 treatments before being able to return to sport relatively pain free. Of the 66 athletes who were able to return to sport, only 3 needed follow-up treatments that consisted of 1-2 additional prolotherapy injections over the course of the follow-up time period (6- 70 months depending on the athlete).

Figure 5. The SI Joint. Image Source12
Switching around to the posterior side of the pelvis, Kim et al examined the effects of dextrose based prolotherapy vs. cortisone (aka – prolotherapy's arch nemesis!) on relieving sacoilliac joint pain in 48 individuals.7 Upon confirmation of SI joint pain following an anesthetic injection, study participants completed 1 month of physical therapy. If physical therapy alone failed to improve symptoms, individuals were randomly assigned to the prolotherapy or cortisone group. Both groups were similar in characteristics at the start of the study; Each had a mean average of 40-44 months of SI joint pain and had similar pain and disability scores.
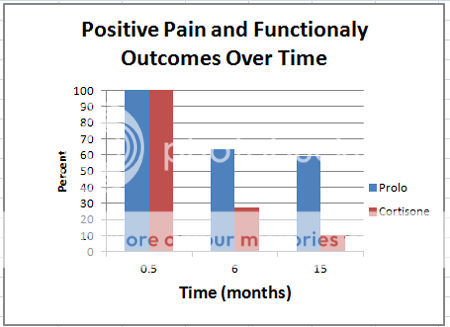
Figure 7. Pain and functionality ODI scores following prolotherapy vs. cortisone injection for SI Joint pain. Data adapted from Kim et al.7 Image created by Sean Casey
Injections were given on biweekly basis for a maximum of 3 visits.7 Using the Oswestry Disability Index (ODI) to assess pain and functionality, > 50% reduction from baseline without having to take any sort of pain medication was considered a success. Upon concluding the trial and tallying up the data, some interesting results were observed by the research team. As seen in Figure 7 both groups had a 100% rate of "clinical successes" in regards to ODI pain and functionality scores 2 weeks following their last injection. However, when assessed 6 and 15 months following the last injection, the success rate for the prolotherapy group remained high while the cortisone group scores plummeted; indicating that prolotherapy may provide better long term relief from SI joint pain.
In a very tightly controlled double blinded study, Yelland et al separated 110 individuals with non-specific back pain into the following 4 groups8:
(Each group had been suffering non-specific back pain for a mean of ~14 years and similar ratings of pain intensity.)
- Dextrose Prolotherapy + Exercise (exercise description rather ambiguous but sounded like 4×10 of birddog/quadruped extensions and 4×10 of curl-up situps per day)
- Saline Injections + Physical Therapy
- Dextrose Prolotherapy + Normal Activity
- Saline Injections + Normal activity
All Saline or Dextrose injections were given at 2 week intervals over the course of the first 3 months. At month 4 and 6, injections were only given if benefit was present. Upon conclusion of the study, each group had ~7 treatment sessions. With respect to improvements, ~55% of each group experienced a > 25% reduction in pain and a > 35% improvement in disability scores at the 12 month mark. Additionally the proportion of those experiencing > 50% reductions for pain and disability did not differ between groups (36-46% for pain; 36-42% for disability). In my opinion, the results found in this study may be explained by one or a combination of the following factors:
- A) Saline isn't a true placebo as it does elicit in inflammatory response (as seen in Part I). Thus, all groups received a prolotherapy-"esque" treatment.
- B) Chronic, non-specific low back pain is a multi-faceted pain beast with various factors leading into it… Were the correct pain generators being treated?
- C) Attention bias – Just having attention from the Physician caused a placebo effect that made them feel better (No control/inactive group was present in study to exclude this factor).
Prolotherapy for the Elbow.
Various studies have examined the effects of prolotherapy for the elbow, specifically lateral epicondylosis (ie – tennis elbow). In slightly less rigorously designed studies, both Carayannopoulos et al.9 as well as Rabago et al.10 have shown patient improvement following prolotherapy treatments. However, rather than spend time hashing out the nitty-gritty results of those studies; I figured I'd shift our focus to a gold standard, double-blind randomized controlled trial study completed by Scarpone et al.11
In their study, Scarpone et al, examined the effects of a dextrose-sodium morrhuate based prolotherapy solution vs. saline solution on pain and strength levels in 20 individual who had failed traditional lateral epicondylosis treatments for > 6 months.11 Measurements of pain (0-10 scale with 10 being "max" pain; 0 being "no" pain), functionality and pain duration did not vary between groups upon randomization. At weeks 0, 4 and 8, study participants received either prolotherapy or saline injection treatments. Following completion of the injection protocol measures of resting elbow pain, grip strength and isometric elbow strength were assessed weeks 0, 8, and 16. At week 52 a follow-up survey was completed by study participants.

Figure 9. Changes in pain levels over time following prolotherapy or saline injections. Data adapted from Scarpone et al. Image created by Sean Casey.
Upon comparing results of the trial, Scarpone found that both groups had improvement vs. baseline.11 However, those receiving prolotherapy tended to fair better and had significantly better long term outcomes. As shown in Figure 9, the prolotherapy group had improvements in pain vs. baseline at all measured time point; this was not observed in the saline group. Likewise improvements in isometric arm extension strength significantly improved at weeks 8 & 16 and again, this was not observed in the saline group.
With respect to the long term impact on completing activities of daily life (ADL), 52 weeks following initial treatments, those receiving prolotherapy fared much better according to surveys:
- 6/10 reported "no pain or impact on ADLs"
- 2/10 reported "mild pain with no impact on ADL"
- 2/10 reported "mild pain and disability with extreme grip only; modest impact on ADLs“
In contrast, those receiving saline only injections reported:
(1 participant did not send back survey)
- 1/9 reported "no pain"
- 8/9 reported "pain sufficient to interfere with ADLs"
Bottom Line
Prolotherapy is a "new", but in all reality "old" treatment, that has just started to gain more steam in the medical community with respect to healing tendon, ligament and cartilage related injuries. As observed in our tour of the human body, various preliminary studies have indicated that prolotherapy may be an effective in this regard.
However, the methodological rigor of the studies has not always been of the highest quality (as defined "by the books"). Furthermore, most of them were small in nature. Until larger studies are conducted, and superior results are shown in them, I feel it will be a little while before prolotherapy is accepted by the main stream medical community (and health insurance plans, at least in the USA, as few cover it as of 2013).
My personal opinion on prolotherapy is that there is enough preliminary evidence to justify exploring this option if you're suffering from connective tissue related pain; Especially if the options are either A) Have Surgery or B) Have Prolotherapy Injections and if fail to experience relief, then explore surgery. When put like this, I think choosing the latter is a no-brainer as it represents a little risk, potentially high reward scenario when using the traditional proliferants (dextrose, sodium morrhuate). And as Part II comes to a close, I leave you with this thought…
Although the potential healing abilities of dextrose and sodium morrhuate based injections are exciting, maybe there is a new frontier in the prolotherapy field, one that magnifies our own body's healing potential many folds above and beyond that which we’ve discussed up to this point; leading to a revolution in the way we go about treating connective tissue injuries…. And maybe that day is closer than what we realize (or maybe still far away!). With that being said stay tuned for final part of our prolotherapy series where we explore the use of Platelet Rich Plasma, Human Growth Hormone, and Regenokine/Orthokine based prolotherapy treatments. In addition, I'll share my personal Re-Search leads to Me-Search experiences with Prolotherapy.
References
1 Fullerton BD.High-resolution ultrasound and magnetic resonance imaging to document tissue repair after prolotherapy: a report of 3 cases. Arch Phys Med Rehabil. 2008 Feb;89(2):377-85. doi: 10.1016/j.apmr.2007.09.017.
2 Yelland MJ, Sweeting KR, Lyftogt JA, Ng SK, Scuffham PA, Evans KA.
Prolotherapy injections and eccentric loading exercises for painful Achilles tendinosis: a randomised trial. Br J Sports Med. 2011 Apr;45(5):421-8. doi: 10.1136/bjsm.2009.057968. Epub 2009 Jun 22.
3 Grote W, Delucia R, Waxman R, Zgierska A, Wilson J, Rabago D. Repair of a complete anterior cruciate tear using prolotherapy: a case report. Int Musculoskelet Med. 2009 Dec 1;31(4):159-165.
4 Dumais R, Benoit C, Dumais A, Babin L, Bordage R, de Arcos C, Allard J, Bélanger M. Effect of regenerative injection therapy on function and pain in patients with knee osteoarthritis: a randomized crossover study. Pain Med. 2012 Aug;13(8):990-9.
5 Rabago D, Zgierska A, Fortney L, Kijowski R, Mundt M, Ryan M, Grettie J, Patterson JJ. Hypertonic dextrose injections (prolotherapy) for knee osteoarthritis: results of a single-arm uncontrolled study with 1-year follow-up. J Altern Complement Med. 2012 Apr;18(4):408-14.
6 Topol GA, Reeves KD.Regenerative injection of elite athletes with career-altering chronic groin pain who fail conservative treatment: a consecutive case series. Am J Phys Med Rehabil. 2008 Nov;87(11):890-902.
7 Kim WM, Lee HG, Jeong CW, Kim CM, Yoon MH. A randomized controlled trial of intra-articular prolotherapy versus steroid injection for sacroiliac joint pain. J Altern Complement Med. 2010 Dec;16(12):1285-90..
8 Yelland MJ, Glasziou PP, Bogduk N, Schluter PJ, McKernon M. Prolotherapy injections, saline injections, and exercises for chronic low-back pain: a randomized trial. Spine (Phila Pa 1976). 2004 Jan 1;29(1):9-16; discussion 16.
9 Carayannopoulos A, Borg-Stein J, Sokolof J, Meleger A, Rosenberg D. Prolotherapy versus corticosteroid injections for the treatment of lateral epicondylosis: a randomized controlled trial. PM R. 2011 Aug;3(8):706-15.
10 Rabago D, Lee KS, Ryan M, Chourasia AO, Sesto ME, Zgierska A, Kijowski R, Grettie J, Wilson J, Miller D. Hypertonic Dextrose and Morrhuate Sodium Injections (Prolotherapy) for Lateral Epicondylosis (Tennis Elbow): Results of a Single-blind, Pilot-Level, Randomized Controlled Trial. Am J Phys Med Rehabil. 2013 Jan 3.
11 Scarpone M, Rabago DP, Zgierska A, Arbogast G, Snell E. The efficacy of prolotherapy for lateral epicondylosis: a pilot study. Clin J Sport Med. 2008 May;18(3):248-54. doi: 10.1097/JSM.0b013e318170fc87.
12 Chris Caldwell. Surgical suite in St. Anthony's Heart and Surgical Pavilion, St. Louis, Missouri. 1 June 2008. This file is licensed under the Creative Commons Attribution 3.0 Unported license. Image accessed May 21, 2013 from: http://commons.wikimedia.org/wiki/File:Samcsurgery.jpg
13 Mikael Häggström. The sacroiliac joint. 14 March 2011. This file is made available under the Creative Commons CC0 1.0 Universal Public Domain Dedication. Image accessed on May 21, 2013 from: https://en.wikipedia.org/wiki/File:Sacroiliac_joint.svg
